The study provides preliminary evidence that certain diabetic and weight-loss drugs have neurological benefits.
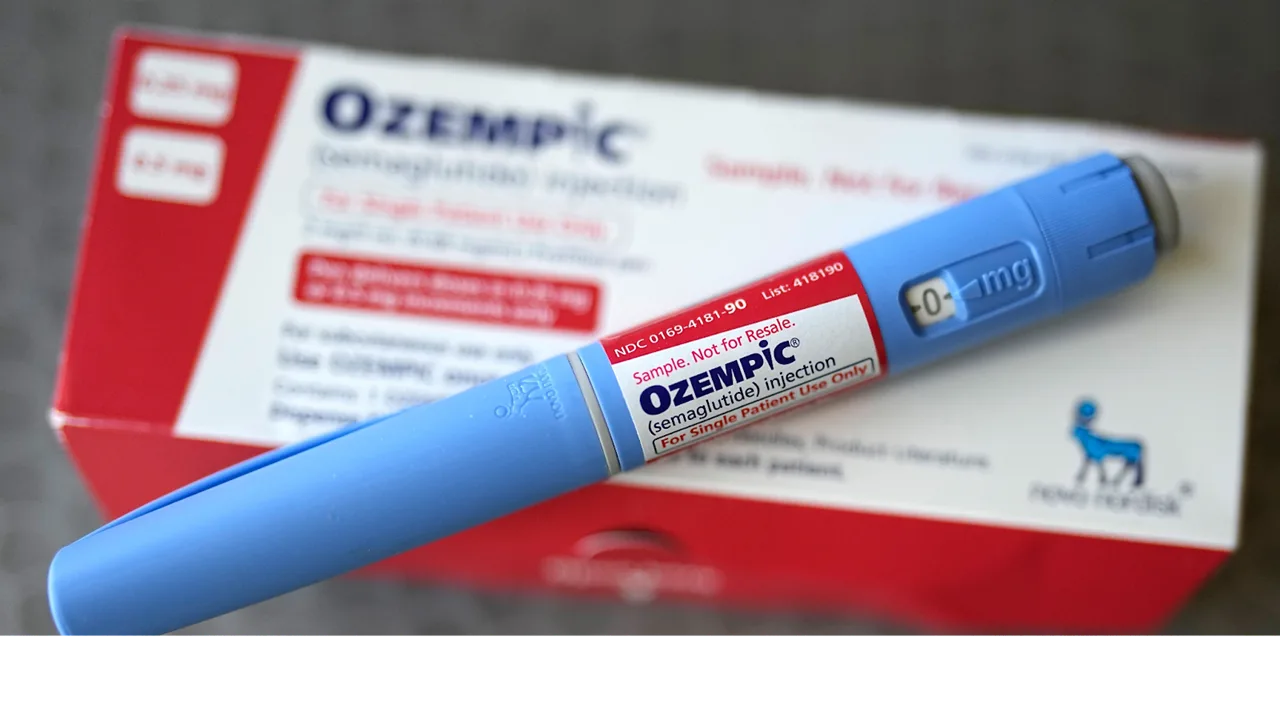
GLP-1 medications may Lower Epilepsy Risk in individuals with type 2 diabetes, according to a recent study. Drugs that mimic the action of the hormone glucagon-like peptide-1 (GLP-1) include semaglutide. Semaglutide, a once-weekly injectable formulation approved for use with diet and exercise in individuals with uncontrolled type 2 diabetes in America, is marketed under the brand name Ozempic. GLP-1 receptor agonists aid in controlling hunger, digestion, and blood sugar levels.
Source:- American Academy of Neurology
Key Details of Lower Epilepsy Risk
| Aspect | Key Details |
| Drug type studied | GLP-1 receptor agonists |
| Common examples | Semaglutide, Liraglutide, Dulaglutide |
| Compared against | DPP-4 inhibitors |
| Study source | American Academy of Neurology |
| Study type | Observational, retrospective |
| Participants | 452,766 people with type 2 diabetes |
| Follow-up period | Minimum 5 years |
| Epilepsy risk reduction | 16% lower with GLP-1 drugs |
| Strongest signal | Semaglutide |
| Key limitation | Not a randomized controlled trial |
Also Read:- Why Doctors Are Recommending 10k Steps a Day Again
The American Academy of Neurology’s medical publication, Neurology, published the findings. It provides preliminary proof that these drugs have neurological benefits. Larger, randomised controlled trials are required to confirm if GLP-1 medications actually prevent epilepsy, even though the results only show a connection.

Also Read:- Why Dates Are the Perfect Mid-Morning Snack for Energy and Immunity
Study Uncovers Epilepsy Risk Reduction
The study’s author, Edy Kornelius, MD, PhD, of Chung Shan Medical University in Taichung, Taiwan, stated, “These results are promising, since people with diabetes are at increased risk for developing epilepsy later in life, but additional randomised, controlled trials that follow people over time are needed to confirm these findings.” Finding strategies to lower this risk is crucial because epilepsy can have numerous negative effects on one’s body, mind, and social life, and many people do not react to the current treatments.”
Researchers used a U.S. health database to analyse patients with type 2 diabetes who had just received a diagnosis and were using either GLP-1 receptor agonists (GLP-1 RAs) or dipeptidyl peptidase-4 inhibitors (DPP-4 inhibitors, or gliptins). None of the individuals had previously been diagnosed with seizures or epilepsy. Dulaglutide, liraglutide, and semaglutide were among the GLP-1 drugs.
Expert Insights and Limitations
“More research is needed, but these findings support the theory that GLP-1 drugs may have neurological benefits beyond controlling blood sugar,” Kornelius stated. “It should be noted that these findings do not imply that DPP-4 inhibitors are harmful in any way or that GLP-1 drugs are definitely beneficial for brain health.”
There are restrictions on the study. Because it is observational and retrospective, unmeasured biases cannot be ruled out. Newer medications, such as tirzepatide (a GLP-1/GIP dual agonist, sold as Mounjaro or Zepbound), were excluded since they were introduced after the study period and are not covered by the findings.
GLP-1 medications increase insulin release, decrease digestion, and reduce appetite by imitating the gut hormone glucagon-like peptide-1. Weight-loss companies like Ozempic (semaglutide) and Wegovy have contributed to their growing popularity, which has raised awareness of additional advantages, such as possible neuroprotective effects observed in animal models for diseases like Parkinson’s and Alzheimer’s.
Key Findings and Methodology
The average age of the 452,766 people the researchers tracked was 61. GLP-1 medications such as dulaglutide, liraglutide, or semaglutide were administered to half of them (226,383). DPP-4 inhibitors were given to the other half. These people were monitored for new diagnoses of epilepsy for a minimum of five years. There was a slight but significant difference between the 1,670 epilepsy cases (2.35%) among GLP-1 users and the 1,886 instances (2.41%) in the DPP-4 group. The risk of epilepsy is somewhat decreased, according to adjusted statistics.
Confounders including age, hypertension, cardiovascular disease, and other comorbidities were taken into account by the researchers. According to the updated results, GLP-1 users were 16% less likely than DPP-4 users to acquire epilepsy.
When the drugs were broken down, semaglutide had the strongest protective signal. Liraglutide and dulaglutide also showed a slight but encouraging trend.
The huge sample and careful adjustments demonstrate credibility in spite of these obstacles. Over 50 million people worldwide suffer from epilepsy, and diabetes is known to increase risk through common routes such inflammation and vascular damage.
Interpretation is further impacted by additional factors such as lacking information on epilepsy risk factors, family history, genetics, alcohol use, or sleep difficulties.
Disclaimer: All of the material in this site, including advice, is general. It is by no means a replacement for a professional medical opinion. For additional information, always speak with a specialist or your physician. This information is not the responsibility of Dietivity.